Join our facebook page for discussions and further good quality learning :
https://www.facebook.com/groups/405813783372378/
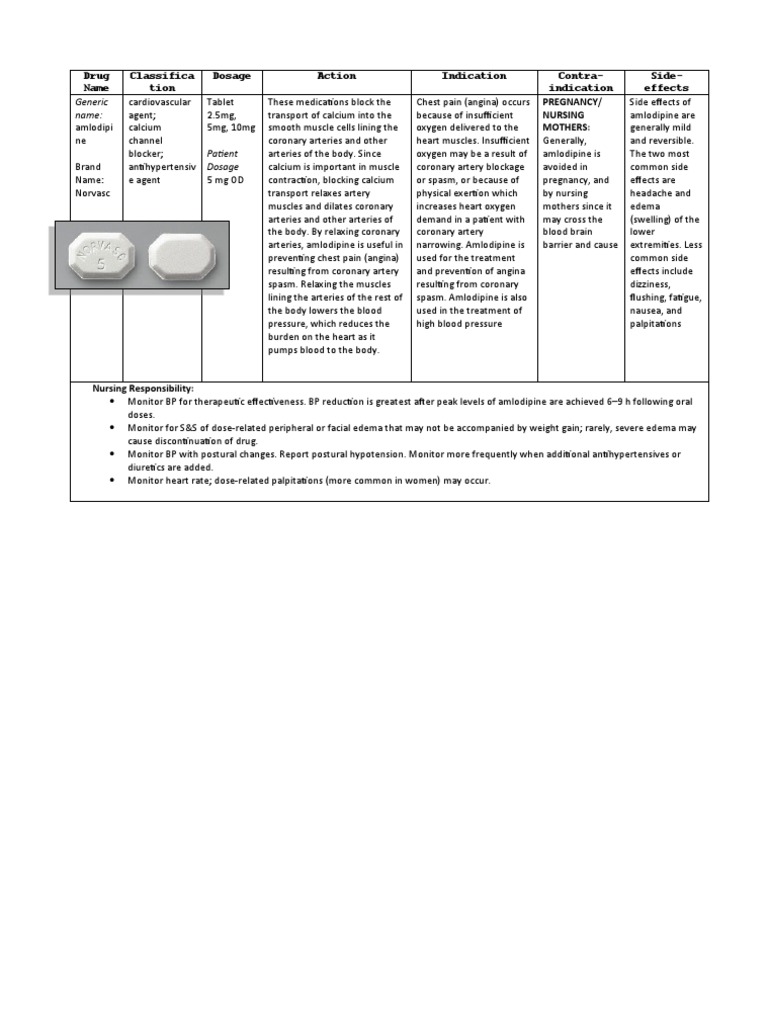
Amlodipine
Mechanism of action :
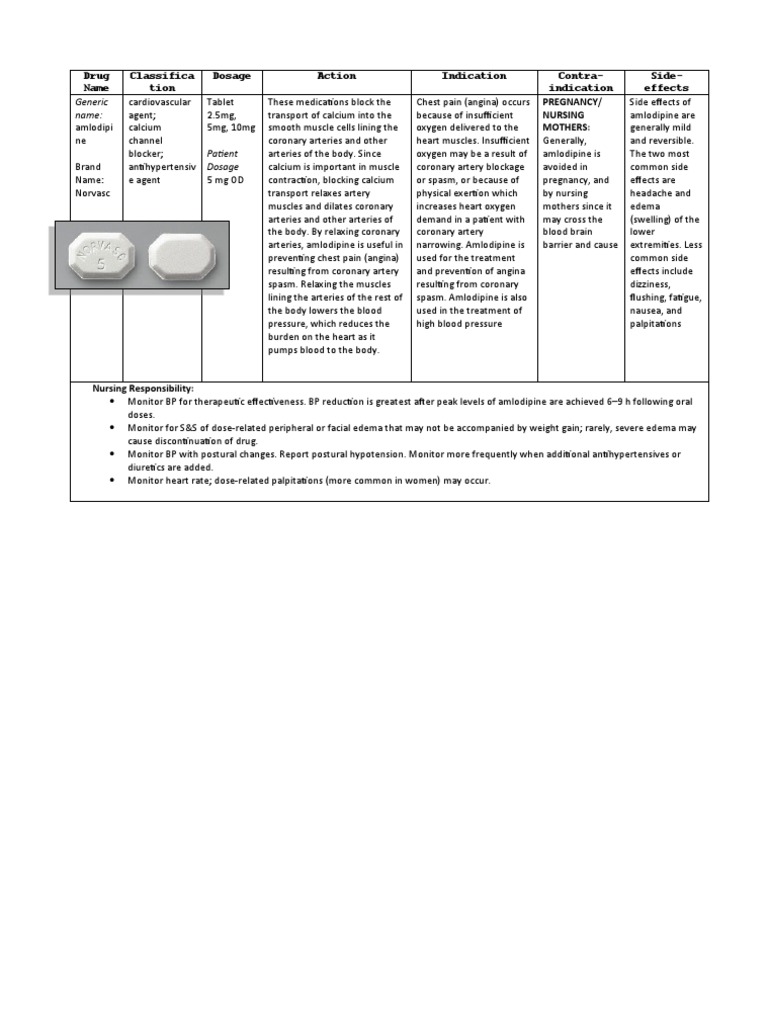
Amlodipine is an angioselective calcium channel blocker and inhibits the movement of calcium ions into vascular smooth muscle cells and cardiac muscle cells which inhibits the contraction of cardiac muscle and vascular smooth muscle cells.
Amlodipine inhibits calcium ion influx across cell membranes, with a greater effect on vascular smooth muscle cells. This causes vasodilation and a reduction in peripheral vascular resistance, thus lowering blood pressure. Its effects on cardiac muscle also prevent excessive constriction in the coronary arteries
 The mechanisms by which amlodipine relieves angina are:
Stable angina:
The mechanisms by which amlodipine relieves angina are:
Stable angina:
Amlodipine reduces the total peripheral resistance (afterload) against which the heart works and reduces the rate pressure product, thereby lowering myocardial oxygen demand, at any given level of exercise.
Variant Angina:
Amlodipine blocks spasm of the coronary arteries and restores blood flow in coronary arteries and arterioles in response to calcium, potassium, epinephrine, serotonin, and thromboxane A2 analog in experimental animal models and in human coronary vessels in vitro.
 Pharmacokinetics
Pharmacokinetics
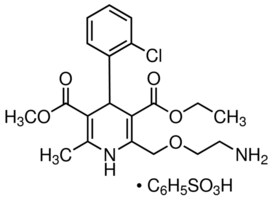
The nitrogen-containing ring is oxidized, and two of the side chains are hydrolyzed.
Amlodipine is well absorbed by the oral route with a mean oral bioavailability around 60%; the half-life of amlodipine is about 30 h to 50 h, and steady-state plasma concentrations are achieved after 7 to 8 days of daily dosing.
Its long half-life and high bioavailability are largely in part of its high pKa (8.6); it is ionized at physiological pH, and thus can strongly attract proteins.
 Side effects :
Side effects :
Some common dose-dependent side effects of amolodipine include vasodilatory effects, peripheral edema, dizziness, palpitations, and flushing.
Peripheral edema (fluid accumulation in the tissues) occurs at rate of 10.8% at a 10-mg dose (versus 0.6% for placebos), and is three times more likely in women than in men.
It causes more dilation in the arterioles and precapillary vessels than the postcapillary vessels and venules.
The increased dilation allows for more blood, which is unable to push through to the relatively constricted postcapillary venules and vessels; the pressure causes much of the plasma to move into the interstitial space.
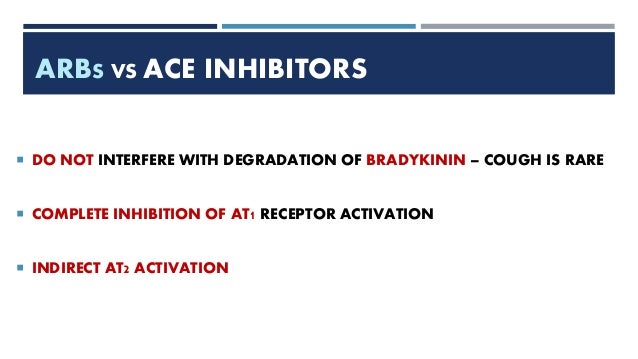
Amlodipine-association edema can be avoided by adding ACE inhibitors or angiontensin II receptor antagonist.
Common but not dose-related side effects are fatigue , nausea , abdominal pain , and somnolence.
Side effects occurring less than 1% of the time include: blood disorders, impotence, depression, peripheral neuropathy, insomnia, tachycardia, gingival enlargement, hepatitis, and jaundice.
 Overdose
Overdose
Amlodipine overdose toxicity can result in widening of blood vessels, severe low blood pressure, and fast heart rate.
Toxicity is generally managed with fluid replacement, monitoring ECG results, vital signs, respiratory system function, glucose levels, kidney function, electrolyte levels, and urine output.Vasopressors are also administered when low blood pressure is not alleviated by fluid resuscitation.
 Combination therapy
Combination therapy
Amlodipine can be given as a combination therapy with a variety of medications:
Amlodipine/atorvastatin, where amlodipine is given for hypertension or CAD and atorvastatin prevents cardiovascular events, or if the person also has high cholesterol.
Amlodipine/aliskiren or amlodipine/aliskiren/hydrochlorothiazide if amlodipine alone cannot reduce blood pressure. Aliskiren is a renin inhibitor, which works to reduce primary hypertension (that with no known cause) by binding to renin and preventing it from initiating the renin–angiotensin system (RAAS) pathway to increase blood pressure.
Hydrochlorothiazide is a diuretic and decreases overall blood volume.
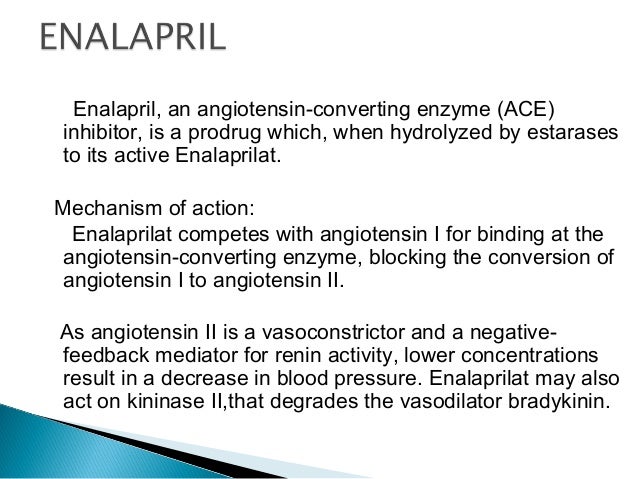
Amlodipine/benazepril if either drug has failed individually, or amlodipine alone caused edema. Benazepril is an ACE inhibitor and blocks the conversion of angiotensin I to angiotensin II in the RAAS pathway.
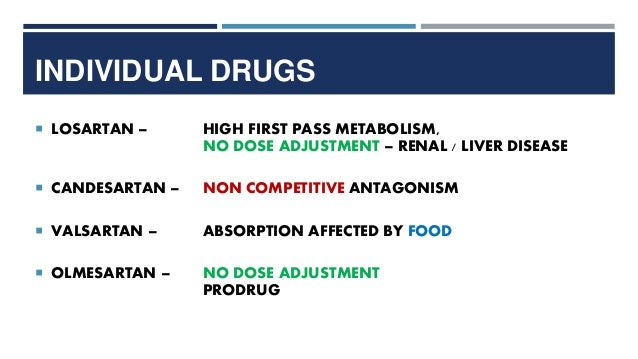
Amlodipine/olmesartan or amlodipine/olmesartan/hydrochlorothiazide if amlodipine is insufficient in reducing blood pressure. Olmesartan is an angiotensin II receptor antagonist and blocks part of the RAAS pathway.
Amlodipine/perindopril if using amlodipine alone caused edema. Perindopril is a long-lasting ACE inhibitor.
Amlodipine/telmisartan, where telmisartan is an angiotensin II receptor antagonist.
Amlodipine/valsartan or amlodipine/valsartan/hydrochlorothiazide, where valsartan is an angiotensin II receptor antagonist.
Contraindications
The only absolute contraindication to amlodipine is an allergy to amlodipine or any other dihydropyridines.
Other situations occur, however, where amlodipine generally should not be used.
In patients with
cardiogenic shock, where the heart's ventricles are not able to pump enough blood, calcium channel blockers exacerbate the situation by preventing the flow of calcium ions into cardiac cells, which is required for the heart to pump.
While use in patients with
aortic stenosis (narrowing of the aorta where it meets the left ventricle) since it does not inhibit the ventricle's function is generally safe, it can still cause collapse in cases of severe stenosis.
In
unstable angina (excluding variant angina), amlodipine can cause a reflex increase in cardiac contractility (how hard the ventricles squeeze) and heart rate, which together increase the demand for oxygen by the heart itself.
Patients with severe
hypotension can have their low blood pressure exacerbated, and patients in heart failure can get pulmonary edema. Those with impaired liver function are unable to metabolize amlodipine to its full extent, giving it a longer half-life.
Amlodipine's safety in pregnancy has not been established, although reproductive toxicity at high doses is known. Whether amlodipine enters the milk of breastfeeding mothers is also unknown.